The coccyx, commonly known as the tailbone, is the tiny bone at the bottom of the sacrum. Funny enough, the tailbone is actually our vestigial tail as it disappears around 8 weeks of gestation. This bone may be tiny but it can play a mighty role in pelvic, low back and even hip pain during pregnancy and postpartum.
What is the Coccyx?
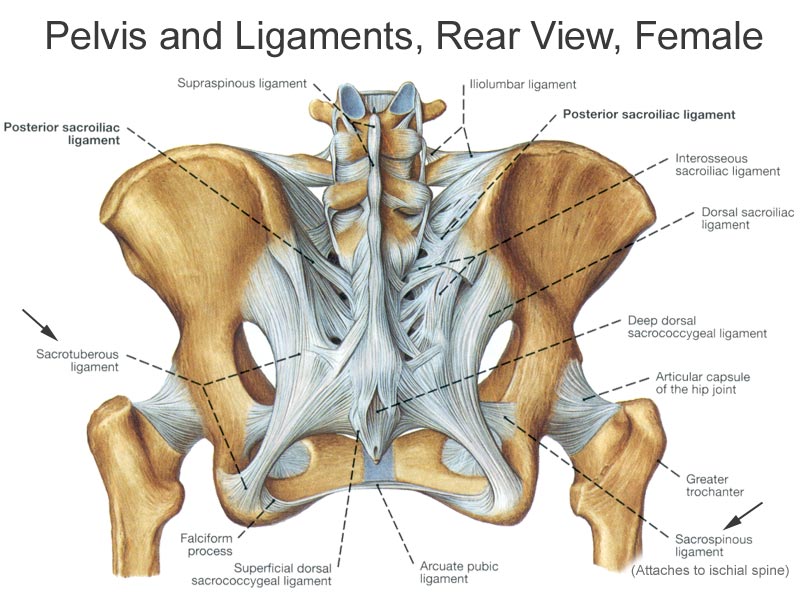
The coccyx is a tiny bone that joins the pelvis at the bottom of the sacrum. This connection is called the sacrococcygeal symphysis and it is supported by five ligaments. Additionally, the coccyx is connected to the anterior longitudinal ligament and supraspinal ligament and these ligaments actually run all the way up to the base of the skull and neck! It is because of it’s mobility and these connections, that many of our movements are done pain-free.
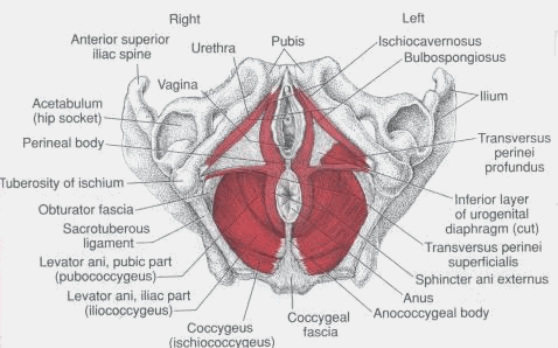
Although it is small, the coccyx also has a lot of little muscle attachments that help to make it a powerful player in the body. On the back side the coccyx connects to the gluteus maximus muscle, the largest and heaviest muscle in the body that helps the hip extend. On the front side the coccyx connects to 10 muscles (5 on each side) which helps create the posterior pelvic floor. It’s connection to the pelvic floor also allows for it to have different positions in men and women. In men the coccyx points anteriorly but in women it actually points downward. This is extremely beneficial in childbirth as is provides extra space for the baby.
Why is the Coccyx Important
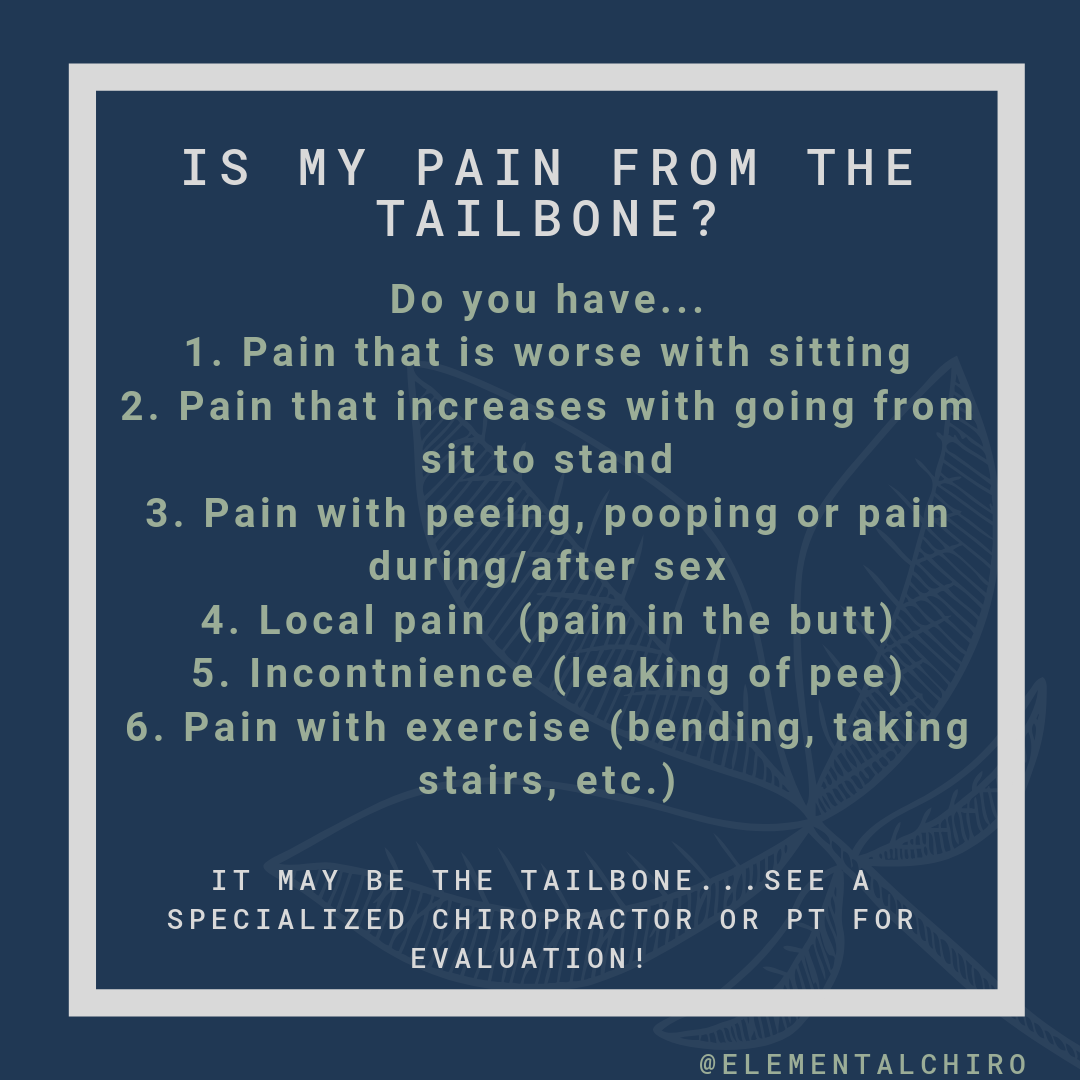
The tailbone is important while sitting as it helps form a tripod support system with the ischium (bony parts under the butt). Sitting on all three points helps distribute weight and creates both balance and stability of the region. This little bone can also move between 5-25º when we move from standing to sitting. (5)
As it connects to the pelvic floor muscles, it also plays a role in pelvic floor stability and strength. The coccyx helps support the anus in order to let us have bowel movements, supports the vagina and even helps us walk, run and move around.
Tailbone Pain during Pregnancy and Postpartum
Unfortunately women are FIVE times more likely to have coccyx pain than men. (2) As it is more common in mamas who have had children, t’s super important to see a prenatal & postpartum trained chiropractor of pelvic floor therapist to determine why you have pain! Besides anatomy and the fact the female coccyx is pointed downward, here are a few reasons why the coccyx may cause pain during pregnancy and postpartum:
Trauma: this includes dislocation or fracture that can happen from repetitive movements (like horseback riding), falls or childbirth. Trauma is also associated with levator ani avulsion which will be discussed during birth trauma down below.
Pregnancy Changes: this may be an easy-out answer but during pregnancy and postpartum the body changes! A few changes most women notice is a change in the low back curve. Many women notice that when they stand they either tuck their butt and clench their glutes or they have an increase low back curve. We also have a change in center of gravity and loss of core strength during pregnancy because our abdominal muscles are literally stretched out in order to make room for the baby.
Baby positioning: if the baby is posterior, this means the bony and hard part of their head is pushing on mama’s sacrum and tailbone. This added pressure (and bony object) on the tailbone can lead to discomfort for mama.
Birth Trauma: whether you had a vaginal or cesarean delivery, the pelvic floor can be affected during childbirth.
During vaginal delivery, 10-30% of women sustain a levator ani muscle avulsion and the use of forceps during delivery can lead to almost 50% of women experiencing a levator ani avulsion.(4) The levator ani is one of the muscles that attaches to the coccyx and is closely related to pelvic organ prolapse. When there is a levator avulsion, part of the muscles are pulled off of the pubic bone. While that sounds a bit scary, the muscle can usually still work even though it is weakened by about 1/3 and can stretch about 50% more than normal.
During vaginal delivery, the muscles and ligaments need to stretch in order to allow the baby out of the birth canal. The process of giving birth inherently destabilizes the low back, sacrum and coccyx in order to allow for this stretching and opening. While opening of the pelvis is essential to childbirth, it may lead to pain if it is not evenly stretched or if it is overstretched.
Use of an epidural has been related to low back pain following both vaginal and cesarean deliveries. A few studies have shown that the use of epidural increases the risk of low back pain from 39% to 52% one day postpartum and 7% to 15% at 6 weeks postpartum. (9) During both deliveries, the body can be in a stressed position; however, the use of an epidural makes it more difficult to recognize stressed positions because the mama can no longer feel the pain and therefore doesn’t know she is in a stressed position and should change positions. Without an epidural the body will have natural protective reflexes that are masked due to the anesthesia. Although counterintuitive, research has shown that the pain related to epidurals may not appear until several weeks after delivery!
Cesarean deliveries are also major abdominal surgeries. It is not uncommon for women to experience pain related to scar tissue adhesions following childbirth. The tissue pull on cesarean scars can be extensive and may actually cause upper and lower back pain or hip discomfort.
Pelvic floor dysfunction: this can be either pelvic floor spasm or weakness or even both! It can also mean the muscles are not coordinated so they aren’t talking with each other at the same time, similar to a game of telephone where the message at the end gets jumbled. This is why it is important to see someone in understanding the pelvic floor who can determine what exactly is going on and therefore lead you to the best results.
Habits: it is important to maintain a neutral spine in both standing and sitting. Mamas frequently have coccyx pain or discomfort after sitting because they roll the pelvis back and sit on the tailbone rather than sitting upright. This is closely related to pregnancy changes and the fact many women have difficulty maintaining a neutral spine while pregnant and postpartum. The same neutral spine we need to sit and stand is what we need to be able to safely lift our children. Often times new mamas are continually bending forward and twisting using their backs rather than their legs and glutes for everyday activities like lifting babies in and out of cribs or carseats or housework like vacuuming and picking up toys. (9)
Referred Pain: the site of pain isn’t always the generator of pain. This is another reason it is important to be evaluated by someone trained in pregnancy and postpartum chiropractic or physical therapy. Coccygeal pain can be referred from the low back and hips, cesarean scar, or even changes in foot mobility!
What Can Be Done to Help Coccyx Pain During Pregnancy & Postpartum (A Conservative Look)?
1. Manual Therapy: you can pick your favorite form of therapy, but everything from deep tissue, manual therapy from a trained chiropractor or PT, dry needling, acupuncture, and visceral mobilization are all options to help relieve coccyx pain. Thanks to all those muscular, ligamentous and tendon attachments, manual therapy of the coccyx can be helpful to reduce pain by restoring the natural movement of the muscles.
2. Pelvic Floor Training: pelvic floor training isn’t just about kegels, it is about the pelvic floor being mobile, stable and coordinated. Even how the coccyx is positioned is important because if it gets pulled to the left, it can actually shorten the pelvic floor muscles on the left while stretching out the pelvic floor muscles on the right. Because this is different for every mama, it is important to determine what is best for you…it may be both relaxing the pelvic floor and strengthening it! Can’t find a local pelvic floor rehab provider but still want help? Check out the “What’s Going on Down There” program which will walk you through a guided self assessment of your pelvic floor!
3. Lifestyle/ Habits: just as our habits can negatively affect our coccyx pain, it is also equally as beneficial in helping coccyx pain. It’s beneficial to keep a neutral spine (gentle, natural curve in low back) when both sitting, standing, getting out of bed, lifting and even using the restroom! In the past sitting on donuts were become recommended for anyone with tailbone pain; however, we have recently learned that sitting on a donut acts as a bandaid and can actually slow down healing by putting the body in a position it normally wouldn’t be in.
Full diaphragmatic breathing and the creation of appropriate intra-abdominal pressure (tension needed to support the body) is also important. Every time we breathe, our abdominal muscles, back muscles, lower ribs, and even pelvic floor should gentle move down and out. This is important because it helps with bowel health by acting like a constant massage, helps to stabilize the low back and naturally stretches and strengthens the pelvic floor. The key is to create pressure and support in 360 degrees and not just downward (that’s bearing down).
4, Exercises: besides breathing, there are exercises you can both add or temporarily take out that may help coccyx pain.
Because of the attachment to the gluteus maximus muscle, it is often important to strengthen this muscle. Some great exercises that activate the glute max efficiently AND effectively are: side lunges, lateral step ups, bird dogs, single leg squat, wall squat, single leg squats and deadlifts, step ups. (3) A fun little fact is that a tight psoas (hip flexor or the muscle in the front of the hip) can actually inhibit the glute max so in these cases it’s equally important to stretch the psoas before activating the glutes.
One thing to determine is what muscles you need stretched vs strengthened. Just because a muscle always feels tight, doesn’t mean it needs stretched. In fact, just as we don’t want to stretch the adductors when we have lightning crotch because it may feel good but can cause the pain to worsen in the long run, we don’t want to overstretch any muscles or stretch muscles that are already long. And the best way to determine what needs stretched vs strengthened is seeing someone trained in understanding these nuances.
If you have been battling with coccyx pain during pregnancy or postpartum, please reach out. Not everyone will fit into these boxes, which is why I am here to help! I love supporting mamas so they can live their best lives without pain.
References:
1. Nathan ST. Fisher BE. Roberts CS. Coccydynia: A Review of Pathoanatomy, Aetiology, Treatment, and Outcome. J Bone Joint Surg [Br] 2010; 92-B: 1622-7.
2. Lirette LS, Chaiban G, Tolba R, Eissa H. Coccydynia: An Overview of the Anatomy, Etiology, and Treatment of Coccyx Pain. The Ochsner Journal. 2014;14(1):84-87.
3. Reiman MP , Bolgla LA, Loudon JK. A literature review of studies evaluating gluteus maximus and gluteus medius activation during rehabilitation exercises. Physiotherapy Theory and Practice. 2012 :28(4): 257-268.
4. Josephine Key. A Movement Problem E-Book: A clinical approach incorporating relevant research and practice 1st Edition .Edinburgh .New York .Churchill Livingstone ELSEVIER.2010
5. Fogel G, Cunningham P, Esses S. Coccygodynia: evaluation and management. J Am Acad Orthop Surg.2004;12:49–54.
6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4418025/
7. ¨Pelvic floor trauma following vaginal delivery. Best Pract Res Clin Obstet Gynaecol. 2005 Dec;19(6):913-24. Epub 2005 Sep
8. https://www.sciencedirect.com/science/article/pii/S0959289X16300887?fbclid=IwAR18IcAs74Xt3Mn-QBd5NEgu9Q68V6yQ6k4B80b90dCRkgzUikfTLbooKJo
9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4845853/?fbclid=IwAR38oSNUj369P8qSGT7cSUwzWcJjgJ9JiWSWc_WuEysEL6DoR5r-ONjsAfs
Disclaimer: The information by Dr. Lauren Keller of Elemental Chiropractic, Inc. is provided for general information only and should in no way be considered as a substitute for medical advice or information about any particular condition. While every effort has been made to ensure that the information is accurate, Dr. Lauren Keller nor Elemental Chiropractic, Inc. make no warranties or representations as to its accuracy and accept no responsibility and cannot guarantee the consequences if individuals choose to rely upon these contents as their sole source of information about a condition and its rehabilitation. If you have any specific questions about any medical matter or think you may be suffering from any medical conditions, you should consult your doctor or other professional healthcare provider. You should never delay seeking medical advice, disregard medical advice, or discontinue medical treatment because of information on this website.