"I had a baby two weeks ago and I feel like I have a golf ball in by vagina."
"I pretty much freaked out when I took a peek down there. It looks like my vagina is swollen and something is coming out."
"I feel totally broken and gross after birth."
"The bones under my butt feel so bruised."
These are all common feelings I hear from mamas after giving birth. If you are freaking out, first take a nice deep breath and know you are not alone. The early postpartum period may not be glamorous but it also doesn’t need to be terrifying.
If you're freaking out about a possible prolapse or incontinence, I get it as I was there too. I see you. I hear you. The best thing to do is not panic (I know, easier said than done) and ask for help.
If you’re anything like me you’re probably thinking, “Why? Why me? What did I do to cause this”
4 reasons you may feel ‘off’ down there after having a baby
1. Here's the thing...our pelvic floors did what they were meant to do! During labor some of our pelvic floor muscles and ligaments lengthened over 3x their normal size to make space for the baby to shimmy into and out of the pelvis. That swelling, pressure, and feeling like a golf ball is in your pants isn't actually a sign of harm or danger in the early postpartum; it's a reminder that it's okay to slow down and let the tissue heal. In fact, in those early days swelling can actually help heal the tissue! Think of it like a nasty ankle sprain..it takes a little bit of time for the swelling to go down and the muscles and ligaments to recover but most people fully recover after some time.
2. During pregnancy your body naturally creates more estrogen which helps make the muscles nice and hydrated so they can easily move. After birth those estrogen levels drastically decrease and can cause irritation, stiffness and pain down there. It takes a few weeks for the hormones to regulate and usually once they do, the pain naturally subsides. There is a catch on this one because if you are breastfeeding it can take up to a year for hormones to fully regulate but there are alternatives like hyaluronic acid or topical estrogen which can help after 6 weeks.
3. Postpartum sleep deprivation is no joke. Unfortunately poor sleep can actually reduce our bodies pain threshold making us even more susceptible to pain. Sleep itself also helps our body heal by releasing hormones to help increase blood flow which sends nutrients and oxygen to the tissue for repair and decreases inflammation.
4. Birth trauma, both physical and emotional can increase pain down there. Physical birth trauma like perineal tears, episiotomies, forceps ro vacuum delivery can all cause pain down there. Pain can also be caused by emotional stressor from birth trauma.
The early postpartum - What can I do to help heal down there?
Often times mamas reach out right after their baby is born freaking out that something is wrong because they might have a prolapse or feel off or they are leaking a little. The first thing I want you to know is that there is a lot of recovery that naturally happens in those first six weeks and you may not even have a prolapse or pain or leaking at your postpartum checkup! With that being said, if you are in the early days or first three weeks postpartum, it doesn't mean you have to struggle through this alone. If you are concerned you might have a prolapse, reach out as there are a lot of things you can do to help relieve the discomfort so you can enjoy this time with your little one.
Five tips to navigate the early postpartum discomfort down there:
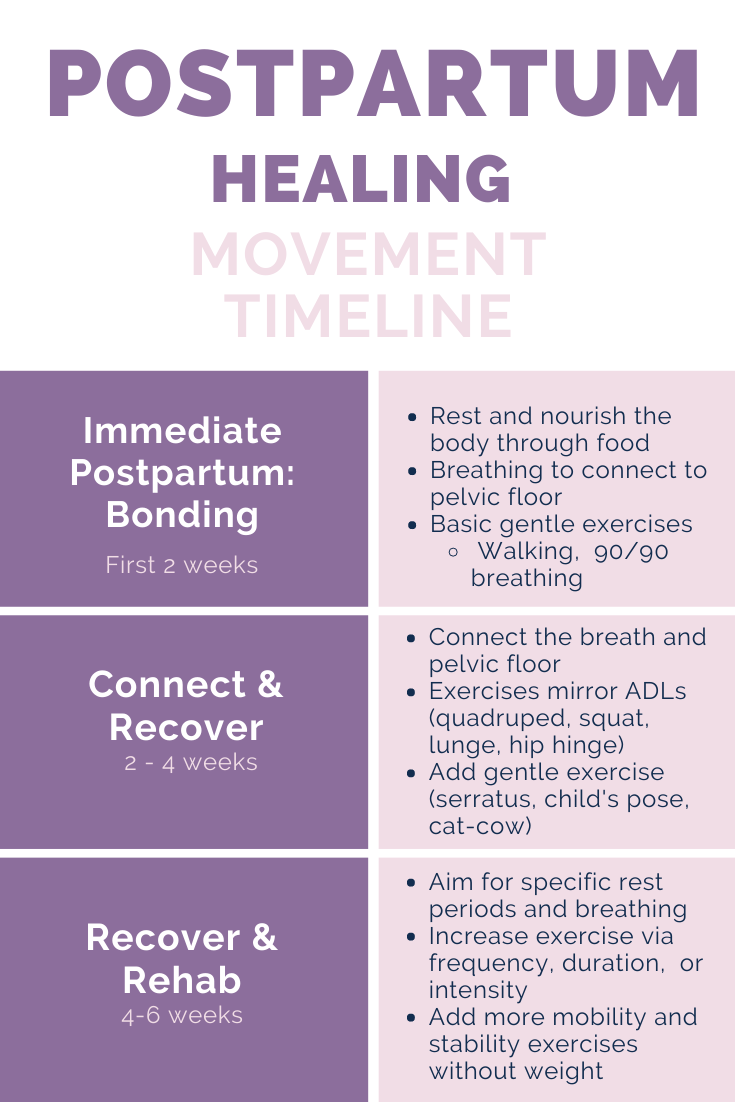
1. Breathe - a deep, full, slow breath that reaches your pelvic floor is a beautiful way to both relax and strengthen the pelvic floor. Aim for 15 minutes a day of focused breathing...this doesn't have to be all at once and ideally you sprinkle it whenever you think about it throughout the day. Breathing is not only a pelvic floor "exercise" but it also increases blood flow into and out of the pelvic floor to help with pain and swelling.
2. Take it easy. If you have older kids this one is hard...there's always housework to be done, toys to pick up and beautiful fun-loving kids to play and snuggle with. If you can, ask for help. Let someone else do the dishes and laundry. Your number one priority is healing and caring for the baby. One way to monitor your activity is by looking at your lochia or bleeding. If you increase your activity level and notice an increase in lochia, slow down.
3. Toilet habits to minimize constipation and straining. That first postpartum poop can be a doozy. Check out this blog to help ease postpartum constipation. Remember to “breathe your poop out” rather than “push your poop” by making low moans and gently breathing.
4. Ice or heat down there. Both have a place in healing postpartum. If you are in pain from perineal tears, a padsicle or ice pack to the perineum may be your BFF to help ease the pain. If you have more muscular tightness then a heating pad or heated rice pack on the perineum or over your low back/butt may be soothing. You can try both and see what it most comforting for you.
5. Reach out for help. If you are in pain or freaking out, you don't need to go through this journey alone. Find a pelvic floor provider who can help you figure out what you need based on your body and your goals. Sometimes the best exercise might be a yoga restorative pose and other times it could look like a deadlift in CrossFit...the key is figuring out what you need.