It’s not uncommon that moms hear that diastasis is only healed via surgery. This information typically comes from a review published in the Surgical Endoscopy in 2017 that stated, “Physiotherapy can achieve a limited reduction in inter-recti distance (IRD) during muscle contraction, though the impact of this finding on patient satisfaction, cosmesis, or function outcome is unclear.” The study, titled The general surgeon’s perspective of rectus diastasis. A systemic review of treatment options was written by all surgeons and compares surgical outcomes to physical therapy outcomes.
What is a “Normal” Diastasis Recti ?
Before looking at the research, it is important to understand what “normal” really means. First, there is a natural, physiological distance between the two rectus mucles. According to Beer, the normal width of the linea alba at 3cm below the umbilicus is 16mm, 22mm 3 cm above the umbilicus and 15mm at the xiphoid in women who have not given birth. Mota stated that for women who have given birth, these numbers can increase to 9-21mm 2cm below the umbilicus, 17-28mm cm above the umbilicus and 12-24mm 5cm above the umbilicus. These values are the normal (not just common) ranges for women who have and have not given birth.
A Critical Look at “The General Surgeon’s Perspective” on Physical Therapy
The General Surgeon’s Perspective article stated that, “Current literature does not describe the successful treatment of DRAM or a reduction of IRD… following physiotherapy.”
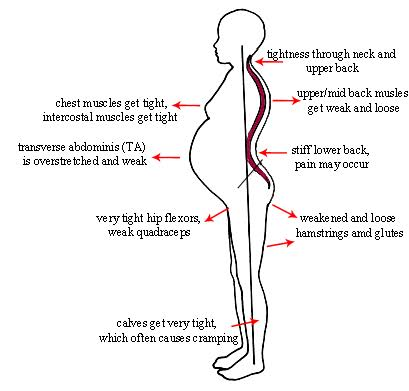
Well, when looking at what the Surgeon General’s states, it appears physical exercise is not a realistic option. The key is to look at what physical exercises were actually performed. Specifically many of the studies included planks, Russian twists, curl-ups, reverse curl-ups and trunk curls. All of these exercises are generally on the list of exercises to AVOID when you have a diastasis. Therefore, the reasoning behind why these exercises were chosen is questionable. This was most notable in the 1st and 2nd study where all of the exercises performed over a 3 month time period are generally contraindicated with a diastasis.
Study #4 showed a 1 fingerbreadth (1.33in/33.78mm) improvement in diastasis recti. The initial evaluation started at less than one month postpartum and only lasted for 2 weeks. Considering that the normal width of a diastasis is 1 fingerbreadth, a decrease from 3.5 to 2.5 finger breadths decrease in 2 weeks (at 6 months postpartum) reflects improvement.
Studies #3, 5, 6 all focus on overall trunk and hip stabilization rather than transverse abdominis or oblique activation. These are also the studies where the measurement of the linea alba at the end of the treatment plan were within the normal range. Although the end results of the diastasis measurements are considered within normal for function, based on the initial starting point, the General Surgeons determined this is not significant.
Surgery for Diastasis Recti
A study published by Akram and Matzen in 2014 in the Journal of Plastic Surgery and Hand Surgery stated that “Rectus diastais is by itself not a true hernia and, therefore, not associated with the risk of strangulation. Repair is mostly done due to cosmetic reasons. The condition does not necessarily require repair.” Furthermore, Akron stated that studies done on abdominoplasty repairs in combination with plication of the linea alba concluded that most evidence is of low quality.
Is Surgery for a Diastasis Recti the Only Option?
My question to you is this, would you immediately jump to surgery for an ankle sprain without trying physical therapy first? The General Surgeon’s article recommends surgery over physical therapy for this musculoskeletal complaint. However, guidelines recommend physical therapy and exercise for a trial of 9 visits over 8 weeks for abdominal sprain. It is possible a diastasis may require surgery down the line; however, surgery should be considered after conservative care/physical exercise has not yielded benefit.
References
- The general surgeon’s perspective of rectus diastasis. A systematic review of treatment options. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5715079/#CR34
- https://www.ncbi.nlm.nih.gov/pubmed/11726260?dopt=Abstract
- https://www.ncbi.nlm.nih.gov/pubmed/14964586?dopt=Abstract
- https://www.ncbi.nlm.nih.gov/pubmed/24256310
- https://www.ncbi.nlm.nih.gov/pubmed/19637295
- https://www.ncbi.nlm.nih.gov/pubmed/29494833
- https://www.ncbi.nlm.nih.gov/pubmed/27475817
Additional Information on the 6 Physical Therapy Reviews listed by the Surgeon General
Here is a review of the physiotherapy reviews:
- Walton, L.M. (2016): After 18 visits (3x/week for 6 weeks) there was a decrease in inter-recti distance from 10.97cm to 6.63cm measured 2cm above and below the umbilicus.
The exercises performed during this program included supine strengthening compared to planks, posterior pelvic tilts, kegels and Russian twists. - Emanuelsson, P. (2016): After 36 visits (3 months, 3x/week for 12 weeks) 87% of the exercise patients were unsatisfied with the results of their training therapy and opted for surgical intervention after completion of the training program.
Exercises included reverse curl ups, v-sits, trunk curls, trunk curls with a twist, and vacuum exercises. - Khandale, S.R. (2016): After 40 sessions (5x/week for 8 weeks, 30 minutes/day) Small decrease in inter-recti distance from 25.3mm to 21.9mm above the umbilicus and 21.9mm to 19.0 mm below the umbilicus.
Exercises included head lift, pelvic lock, plank, superman and double leg raise. - Acharry, N. (2015): After 4 sessions (2x/day for 2 weeks) Starting at less than one month postpartum, decrease in inter-recti distance from 3.5 fingerbreadths to 2.5 after 2 weeks.
Exercises included head lift, pelvic tilt, and pelvic clock with bracing. - Litos, K. (2014): After 18 sessions (2x/week over 16 weeks) Case report starting 7 weeks postpartum to 4 months postpartum, inter-recti decrease from 11.5cm to 2cm and improvement of patient-specific functional scale from 4/30 to 30/30.
Exercises included core stabilization exercises and strengthening of the hip and trunk muscles, including standing “wall hold”, shoulder curl-up with bracing, modified plank with TA hold, birddog, lunge walk holding 10lbs weight, bosu lunges, bosu alphabet, squats with 4lbs, overhead squat. - Sheppard, S. (1996): Unknown sessions started 2 years postpartum an re-checked 4 months later. The inter-recti distance decreased from 60mm to 7mm.
Exercise included prone-kneeling.