Full disclaimer, this is probably one of the nerdiest posts I have ever written, but I think it's important for more people to understand. If you're in Neurodivergent support groups, you've probably seen:
“My child refuses to potty train”
“My child won't pee/poop on the toilet”
“They don't tell me when they need to go”
“It's like my child doesn't care if they sit in their pee or poop”
As a pediatric pelvic floor provider, I usually want to shout from the mountain tops and explain that it isn't a won't/doesn't care situation as much as a “I'm struggling to learn a task” and need more or different support. And since I'm a WHY person, I want to take the time to help other people understand why Neurodivergent kids may struggle with bowel and bladder issues.
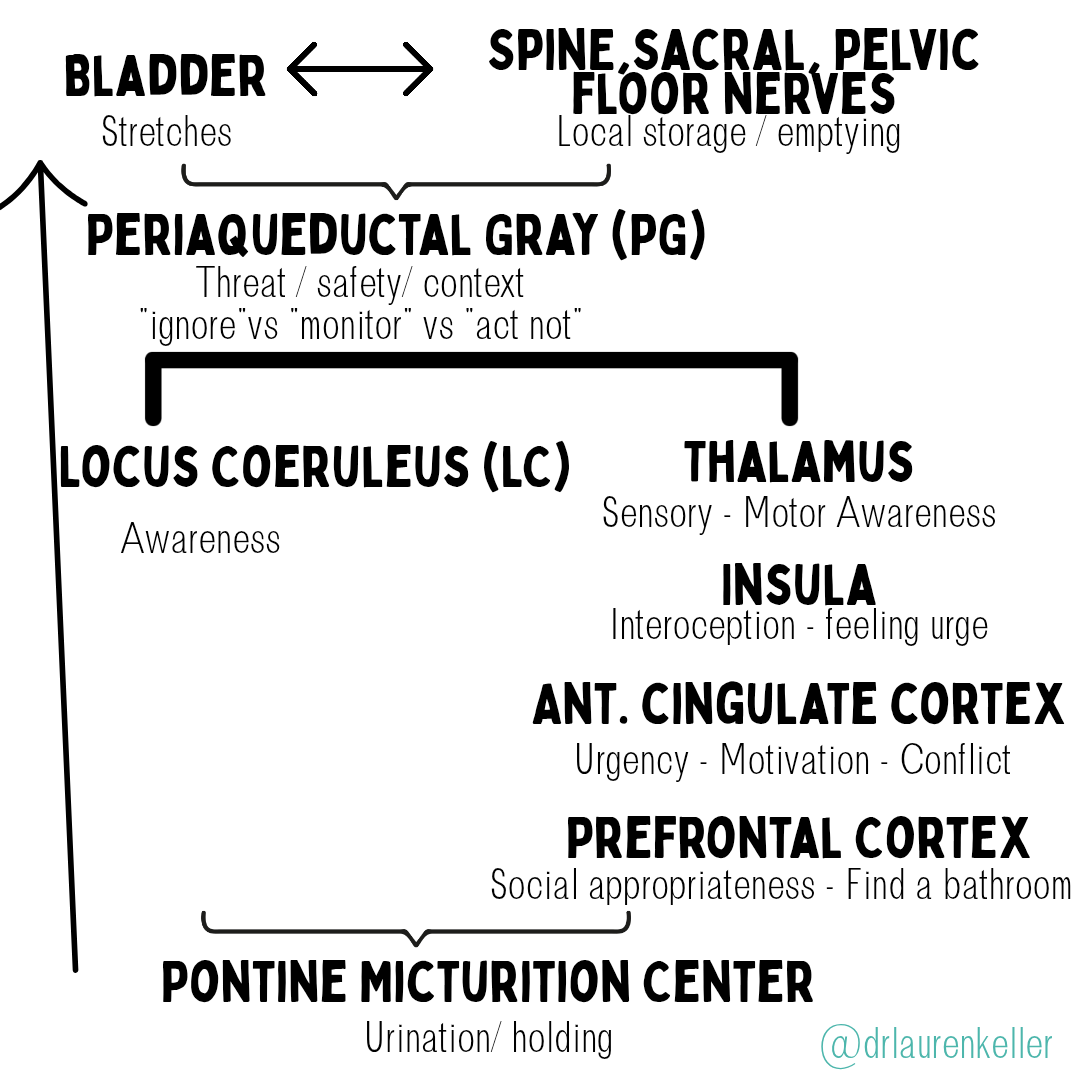
First, let's talk about how we know when we have to pee. As we move throughout the day, our bladder fills with urine. Once the bladder stretches a certain amount, the bladder sends a signal to the brain. This signal is based on bladder pressure or how much urine is in the bladder.
In newborns and young children the brain isn't fully developed and it simply empties automatically once full…that's why we have diapers. As children get older and their brains mature, this is when we develop the nervous system control that allows for bowel and bladder training.
One part of the brain (the periaqueductal gray or PAG) recognizes that stretch and determines if you are going to ignore it or act on it. This area of the brain also processes threats (fight/flight/freeze), modulates pain (determines if there is or isn't pain), and is in control of breathing, heart rate, supports REM sleep and temperature regulation along with urination. I highlight these other actions of the PAG because a lot of Neurodivergent people will recognize that they (or their children) may process one or more of these other aspects differently…from sensory sensitivities, differences in pain perception (hypersensitive vs hyposensitive), sleep differences to emotional regulation. While more research is needed, we have a few studies that have shown that Autistic people have increased brain volume and density in this area. One thing we frequently talk about is co-regulation and helping children feel safe in their environment based on how their brain processes that information. When it comes to the restroom, if a child is in pain (from constipation or bladder spasms), overwhelmed by sensory information or afraid of what might happen (Will they fall into the toilet? Will the toilet suck them down the drain?), then the body will prioritize the threat over the need to use the restroom. The changes in the PAG and its ability to determine threat and safety is one reason Neurodivergent people process the need for urination/defecation differently.
From the PAG, the sensory relay system next goes to two parts of the brain – the locus coeruleus (LC) and thalamus sensory relay. The LC is in charge of arousal/alertness. The LC is heavily studied around sleep because of the role it plays in alertness…or how the body responds to a stimulus. When it comes to the bladder, the LC is what says “this is important and you need to take action now” or “nope, this is background noise, no need to pay attention” or “you might want to start paying attention to this.” It also is in charge of norepinephrine, which is frequently considered the fight/flight/freeze hormone. The LC quite literally tells you to pay attention. As an adult, if you've ever been so focused on something (hyperfocused or time blindness) that you've forgotten to eat, drink, or pee, it's the LC that prevented those sensations from coming to consciousness. For kids, this is the child that is playing a game and doesn't realize they need to use the restroom because their brain is focused on the game and hasn't prioritized the need to pee/poop. If there is pain or discomfort with urination, the body will also increase its norepinephrine response…which can decrease body awareness, and increase pelvic floor tone. This is where pediatric pelvic floor therapy excels because it can work on decreasing the threat response.
At the same time the LC is doing its job, the sensory signals go to the thalamus on its way to the insula, ACC, PFC. The thalamus is the sensory and motor relay system…every single sensation we feel or movement we do goes through the thalamus. From the thalamus, the information goes to the insula. If you've been in the Neuroaffirming community long, you've probably heard about interoception- or the body's ability to feel bodily sensations…from hunger, thirst, bowel and bladder to a racing heart. The insula is the part of the brain that processes interoception and builds body-sensation vocabulary. It's the part of the brain that says “I feel pressure in my lower abdomen. That means I need to pee.” It's what connects the sensation to what it means. Research has shown reduced activation in the insula in autistic and ADHD children…meaning that they frequently have both decreased sensation (interoception) and decreased connection to meaning. This is highlighted by children who “don't feel the urge to pee/poop” as well as by children that may do the “potty dance” but they don't recognize they need to use the restroom.
From the insula, the bladder sensations move to the anterior cingulate cortex (ACC). The ACC frequently has both a different structure and altered connectivity in ADHD and autistic people. This area of the brain is what processes urgency, motivation and conflict detection. This is seen in the child that doesn't recognize the urge until it's too late…the child that jumps up and shouts, “I need to go NOW!” When it comes to motivation, this is the child that may recognize they need to go, but their brain says, “Nope, this isn't important enough to act on” or the brain says, “I am too busy”. When it comes to Pathological Demand Avoidance (PDA), this is the area of the brain that says, “This is too many demands. We are under attack, and instead of using the restroom, we are going to hold our pee and avoid it at all costs.” A child isn't refusing to use the bathroom, their brain has determined that the bathroom is a threat to their safety and is avoiding it to try and limit threats/demands.
Another part of the brain, the prefrontal cortex, “reads the room” and determines if it is a socially acceptable time to use the restroom.
If you're in a bathroom, then your brain tells your bladder that it is okay to go. If you're not in the bathroom, your brain tells your bladder it needs to wait until you can find a restroom. The bladder continues to fill until you can make it to the restroom.
After the LC and thalamus sensory route, the sensory relay system goes to the Pontine Micturition Center (PMC). The PMC is in charge of finally giving the “go” signal and allowing the bladder to physically go. While it is in charge of supporting bladder filling and preventing leaking, the PMC does NOT decide whether or not this happens…it simply reacts to what the other parts of the brain tells it to do.
Now, let's go back to the beginning for a minute. Remember how the bladder starts the signalling process by reaching a certain pressure? To make it easy, let's look at a 10-year old's bladder. They normally respond when there is ~250mL (~1 cup) inside the bladder. Let's think back to all of the parts of the brain that could over-respond or under-respond and lead to a person not using the restroom or using the restroom too frequently! When urination is delayed, the bladder will naturally start to stretch more and the brain may say, “we don't need to respond at 250mL, let's wait until it's 450mL” and over time that becomes 500mL. The bladder capacity can quite literally double. When this happens, it can cause pain whenever the bladder contracts or whenever they go pee…leading to increased pain/discomfort or decreased safety. This can lead to a cycle where the body has learned it is not safe to pee or poop so kids withhold to keep them safe. This isn't behavioral…it's a safety response!
Now, take a deep breath and let it all out. I know that was a lot. But if there is one key takeaway from this, it's to focus on supporting your child and their brain so you can help them learn their body's signals and brain's safety measures to help them feel safe in the bathroom.