Pregnancy Tips to Help You Prepare for Birth
Pregnancy is an amazing time when our bodies are going through a wild ride of transitions from bloating and constipation to swollen feet and possibly even fear of the unknown. It’s also a time that we are creating a beautiful life that we will soon welcome. Even with the hiccups in life, that doesn’t mean we need to succumb to the negatives! In fact, I believe that pregnancy should be (mostly) enjoyable. Here are my top 7 pregnancy tips:
Focus on Core Strength & BREATHING
To improve core strength means you are also improving pelvic girdle strength and helping cultivate a strong pelvic floor that is able to dynamically move through labor and delivery. The core is naturally activated through proper diaphragmatic breathing and moves in connection with the diaphragm and pelvic floor to help RELAX the pelvic floor. Being able to appropriately activate and relax the pelvic floor is important during labor because it may decrease 3rd and 4th degree tears and the need for an episiotomy! Another added bonus is that working on core strength during pregnancy can speed up the recovery of diastasis postpartum.
Avoid Constipation during Pregnancy
I know this is about postpartum constipation, but the 5 of the 6 suggestions (+ the bonus) all may help relieve constipation during pregnancy. So go ahead, eat more veggies, stay hydrated and don’t hesitate to buy one of the best inventions ever, the Squatty Potty. Avoiding constipation can relieve pressure on the pelvic floor that can lead to dysfunction later on. Plus, who doesn’t love a daily BM?
See Pelvic Floor Specialist AND a Chiropractor during Pregnancy
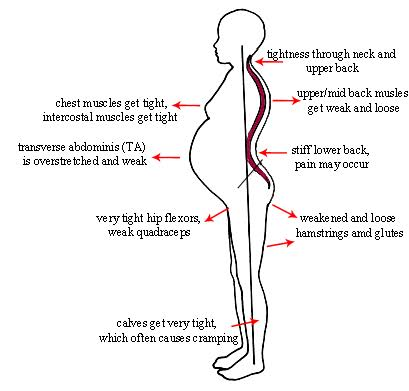
For some reason think this is an OR situation but what better way to move through pregnancy than optimizing your body through functional movements and adjustments? I love when mamas see both me and pelvic floor therapist to get the best outcome for their pregnancy. In my opinion, this is one of the best ways for a mama to prepare for birth because it helps her mobilize and stabilize her body in order to support the structural changes that come with pregnancy, delivery and postpartum.
Continue or Start Working out / Train for birth
Training for birth isn’t about reaching new PRs or hitting every gym day at full intensity. It’s about nourishing the body through movement and listening to your body’s needs. It’s about mobilizing the body so it can move optimally while also being strong. Working out during pregnancy can even include learning different positions that can be used during labor and delivery that can help ease pain and keep you moving.
Take a Childbirth Education Class
Did you know the first stage of labor could take Taking a class can help you prepare for the unknown and plan for it. That way when the time comes you aren’t surprised about the changes coming your way. Planning ahead can help you prepare for the birth you desire and just as important, create a backup plan for if things don’t go as planned. Having your ideal plan and working through decisions before you are in pain and possibly scared can be really empowering so you feel you get to make an educated decision!
Hire a Doula
Full disclosure, I am biased towards a doula. I love doulas because they are able to offer emotional support and knowledge in labor to help a mama move through the delivery process. Even with a supportive partner, a labor doula can help a mama know what to except and calm any nerves that may arise during labor.
Listen to and Respect Your Body
Learn from my mistakes, please! When I was pregnant with my first I had this attitude that I was strong enough to do anything and slowing down was a sign of weakness. I literally worked an eight hour shift with zero breaks and I ate a handful of nuts while in the restroom one day. My idea back then was that strength was determined by how much I physically accomplished. If I was tired, I pushed through. If I was hungry, I held off eating until my next break. I wasn’t going to be weak and take the breaks my body was craving. Sure, I was accomplishing a lot of tasks but I was left physically and emotionally drained. This time around one of my main goals is to listen to my body and respect what it needs. Some days this means eating more food, some days it is resting more and other days I feel comfortable and confident enough to do everything. I know it’s still early in pregnancy but I already feel physically and mentally better because my soul isn’t constantly exhausted trying to check off all of the boxes. So, do what you need to do to fuel your body- that can be rest, less or more activity, less or more food, maybe it’s doing the Expectful app daily and maybe it’s doing more yoga. Each person is different and each mama’s needs can change day-by-day so tune in and check your own needs daily.